
NYHealth's "Best of 2022" Annual Report
In 2022, the worst of the COVID-19 pandemic was finally behind us. NYHealth focused on connecting New Yorkers to healthy food; empowering health care consumers; improving veterans’ health; and responding to time-sensitive and emerging health issues. Explore our Best of 2022 to learn about some of our biggest wins.Connecting New Yorkers to Healthy Food
Connecting New Yorkers to Healthy Food
To ensure New Yorkers have the food they need to thrive, there is no substitute for listening to the voices of those who are directly affected by hunger. As a first step, we developed and commissioned the first-ever statewide survey on food and health in New York State. The survey dives deep into the connections between food and New Yorkers’ health, why obtaining and preparing food can be difficult, and the perilous tradeoffs people make to put food on the table. We also issued related briefs on food insecurity in families with children and the differing experiences with food insecurity among rural, urban, and suburban New Yorkers.
The survey results show wide support for policies to reduce food insecurity and improve health, including universal free school meals, streamlined benefits applications for public programs, and the use of Supplemental Nutrition Assistance Program (SNAP) benefits to purchase groceries online.

NYHealth grantees launched new projects, expanded their work, and leveraged our support to reach more New Yorkers in each of our Healthy Food, Healthy Lives strategies: healthy food systems planning and capacity-building; nutrition benefit programs; healthier, culturally responsive food in public institutions; and Food Is Medicine:
- Farm to Table is providing a cohort of our food systems planning grantees with expert capacity-building support to advance their local and regional plans. With this support, the cohort will be able to accelerate and improve their plans, integrate those efforts into a coordinated body of work to align policies, and ultimately drive a master food systems plan for all of New York State. And some of these grantees have already made impressive strides in leveraging our initial investments to support and sustain their work. Using a modest NYHealth grant, Black Farmers United NYS launched a statewide campaign to help Black farmers advance solutions for racial equity in agriculture and healthy food. New York State has now included $200,000 in its 2023 budget for Black Farmers United NYS in support of its efforts. Newburgh Urban Farm and Food Initiative received a $200,000 planning grant from the USDA to support its resident ambassador program, encouraging residents to learn more about urban farming and the importance of local food systems.
- Field & Fork Network continued its statewide expansion of its Double Up Food Bucks program, which lets SNAP recipients use their benefits and receive a matching value on dollars spent on fresh produce at participating farmers markets, mobile markets, and corner stores. Field & Fork Network secured a $2 million annual appropriation from the State to expand the program, and it also has an opportunity to leverage an additional $2 million in federal funding, for a total of $4 million going directly to New York State farmers and local economies. The program is now operating in 32 counties and serving 32,000 SNAP recipients, giving more families with low incomes better access to healthy, local food. More than 20 grocery stores across the State also accept Double Up Food Bucks—all of which are required to source at least 15% of fresh produce from New York State farms. At the close of 2022, the program surpassed $1 million in healthy food sales for the first time in New York State.
- Lenox Hill Neighborhood House (LHNH) continues to scale its successful farm-to-institution training program, The Teaching Kitchen, beyond New York City. Offered for free, the program is a nuts-and-bolts course that helps nonprofit food service organizations serve more healthy, fresh, and local food—without raising costs. Building on our previous investments to expand the program, LHNH trained food service staff in 20 Hudson Valley school districts over 2022; as a result, more than 4,000 school children in the region will have access to more nutritious meals. American Farmland Trust released its Farmer Readiness Scan tool, designed to help New York farmers, growers, and producers identify challenges and barriers to institutional procurement, receive feedback toward successfully selling wholesale to institutions in New York State, and demystify the farm-to-school procurement process. The tool will build and foster better connections between farmers and school food teams that make their school food decisions.
- NYC Health + Hospitals began piloting Food for Health, a home-delivered fruit and vegetable prescription program for families with young children—the first of its kind in the nation. To date, more than 170 families living on low incomes have enrolled, and initial feedback from the participants indicates they are consuming healthier produce.
NYHealth’s four strategies for connecting people to healthy food were also reflected in the goals of the historic White House Conference on Hunger, Nutrition, and Health held in September. We worked with the funder community to identify key action steps that funders could take in the planning and follow-up to the historic conference. We also see synergy with the USDA’s agenda for nutrition security. NYHealth’s inaugural Healthy Food, Healthy Lives conference in March featured keynote speaker Dr. Sara Bleich, Director of Nutrition Security and Health Equity at the USDA, as well as two panels with our grantees and other experts that highlighted federal and State actions that can have a positive impact on New York’s food future.
Meeting the Needs of Veterans
Meeting the Needs of Veterans
The rate of veteran suicide in New York State has started to stabilize in recent years, signaling that perhaps the State’s efforts to prevent veteran suicide may be working. However, more work needs to be done; a recent NYHealth brief shows the need for interventions to address higher rates of suicide among younger veterans and the dramatic increases in the use of firearms as the method for veteran suicide in New York State.
In 2022, NYHealth continued to support suicide prevention programs and share what we’re learning through public testimony and publications. Peer mentoring programs are a proven and effective factor in suicide prevention interventions; NYHealth has made numerous investments in these programs that are starting to bear fruit. Western New York Heroes conducted outreach and enrolled more than 300 veterans to participate in its flagship peer mentoring programs, Operation B.O.O.T.S. and Heroes Bridge. The Veterans Outreach Center recruited 353 veterans to participate in tailored programs and connect them to community resources, including support groups and trauma recovery services. The Steven A. Cohen Military Family Center at NYU Langone continued its work to provide high-quality telemental health services and peer support to post-9/11 veterans in hard-to-reach, under-resourced areas of New York State, such as the Southern Tier and North Country regions, and served nearly 400 veterans in 2022. New York Cares recruited and trained 126 volunteers to provide “buddy checks” through telephone outreach to veterans in need. ETS worked to expand the reach of its peer mentor program into New York City and 13 counties in the Finger Lakes region, reaching more than 250 veterans. Leveraging the $20 million State investment to expand the successful Joseph P. Dwyer Peer Support Program across New York, long-time NYHealth partner D’Aniello Institute for Veterans and Military Families (IVMF) at Syracuse University is developing policy recommendations that could strengthen this effective program and better support military veterans. NYHealth also leveraged a $750,000 federal investment in the Veterans One-stop Center of WNY to help expand its services into four additional counties, supporting targeted outreach that will connect additional veterans with comprehensive services.

We know that a strong Department of Veterans’ Services (DVS) is vital to supporting the 600,000 veterans that reside in New York State. NYHealth had previously supported a report from IVMF that examined divisions of veterans’ services across all states to highlight successful and unique approaches to supporting veterans. The report laid out specific recommendations for how New York State could strengthen its DVS. In 2022, the State Division of Veterans’ Services was officially elevated to a department status—a direct result of the report’s recommendations and a significant win for New York State’s veterans. In response, we outlined the steps that still need to be taken in an op-ed and hosted a webinar with the new Director of DVS, Reverend Viviana DeCohen.
Placing Patients at the Center of the Health Care System
Placing Patients at the Center of the Health Care System
Too often, patients are marginalized rather than placed at the center of the health care system and treated as its most important customers. Promoting information transparency and engaging patients as partners in health care decision-making can empower consumers to make better health care decisions and to have a voice in the health care system.
Shared visit notes, often referred to as open notes, help patients become active participants in their own care. Building on our longstanding work to help spread open notes throughout New York State, we selected 16 hospitals from across the State for grants totaling nearly $800,000 to support them in sharing open notes in compliance with recent federal information-sharing requirements. As part of our partnership with the OpenNotes national program office, these hospitals now have the funding, technical assistance, and peer-learning opportunities to implement and share open notes more effectively with their patients. For example, Mount Sinai Health System in New York City is educating its providers on appropriate, patient-friendly documentation, including strategies to counter bias in health care information, as part of its project. Upstate University Hospital in Syracuse is launching marketing and patient engagement campaigns and training providers on using notes for shared decision-making. As a final prong in this effort, we released a Request for Proposals in November for federally qualified health centers, private physician practices, and other non-hospital systems to support open notes implementation and patient engagement. Applications must be completed and submitted by January 26, 2023, and grantees will be announced in spring 2023.
Seasoned health care advocates as well as patients who are newly speaking up about their own care experiences are driving policy changes to create a more patient-centered health system. On the issue of medical debt, for example, Health Care for All New York called upon its strong and wide-ranging coalition of consumer advocates. Community Service Society of New York’s We the Patients NY Campaign activated and elevated the voice of patients through social media. The End Medical Debt in New York Campaign mobilized communities across New York State in grassroots organizing. And significant policy wins for health care consumers in New York State are now steadily notching up. In November, Governor Hochul signed into law a measure to prohibit the extreme billing practice of placing liens on patients’ homes and garnishing wages. And in December, Governor Hochul signed legislation banning hospital facility fees for preventive care and requiring advance notice to consumers for instances in which fees will be charged. New partners have also joined the mix to build on momentum and get key medical debt protection policies across the finish line. Volunteer Lawyers Project of Central New York is providing legal expertise to advocacy efforts and on-the-ground assistance to consumers. Separately, the Urban Institute is studying credit data to provide a clearer and more comprehensive picture of medical debt patterns across New York State.
Another major consumer-focused policy victory in 2022 was the confirmation of a second consumer representative to serve on the New York State Public Health and Health Planning Council, which reviews hospital transactions like mergers and closures. This achievement is a culmination of efforts by our grantee Community Catalyst and statewide partners in the Community Voices for Health System Accountability coalition to help New Yorkers and communities play larger roles in the State’s oversight and regulation of health facilities. These advocates are also playing an instrumental role in making a consumer-focused policy win from last year a reality. They are providing recommendations to policymakers on how to assess the equity impact of hospital mergers on marginalized patient populations as part of their oversight, following a requirement Governor Hochul signed into law in 2021. Community Catalyst and other partners shared best practices, models, and tools for effective consumer engagement and advocacy across New York State at a webinar in December.

Telehealth emerged as a critical option for patients early in the pandemic, and it’s here to stay. But people of color, people with low incomes, those who speak a primary language other than English, older adults, and rural residents face numerous barriers to telehealth use. New York City Health + Hospitals, AIRnyc, and EngageWell Independent Practice Association are developing replicable patient navigation models to make telehealth services more effective and equitable for New Yorkers. These models have demonstrated the value of telehealth in improving patient experience and health care utilization, as shared in an NYHealth webinar and in national, peer-reviewed publications.
Our Patients as Partners: Advancing Equity grantees are also making strides in developing educational resources, care models, and practice improvements designed to place patients of color at the center of their health care experience. For example, FAIR Health launched a suite of decision-aid tools that, for the first time, pairs treatment and cost options for conditions disproportionately impacting people of color. Users have visited the webpage housing these tools more than 10,000 times. And with the help of a learning collaborative led by the Center for Health Care Strategies, health systems across the State have implemented equity-focused patient engagement and quality improvement initiatives that, for instance, have reduced no-show rates for pediatric appointments. A toolkit shares lessons learned from these health systems’ efforts and offers actionable steps for providers.
NYHealth wound down our Empowering Health Care Consumers program at the end of 2022, having largely accomplished our goals, thanks to the dedication and effectiveness of our grantees. Over the last six years in this program area, we invested nearly $19.5 million in support of more than 150 projects to promote information transparency and engage patients as partners both in their own health care and at the policy level. Although the work of empowering consumers will never fully be done, there’s a solid foundation in place from which to grow the burgeoning efforts of consumer advocates and organizations across the State.
Responsive Grantmaking
Responsive Grantmaking
In many ways, 2022 was turbulent; numerous public health crises emerged in New York throughout the year. NYHealth responded nimbly, quickly, and flexibly to a number of these emerging issues. The Foundation also seized new and timely opportunities to address ongoing public health and health care system challenges.
Emergency Needs
As the mpox (monkeypox) health emergency became dire in New York City, NYHealth worked with Callen Lorde to provide outreach and education to nearly 60,000 New Yorkers at risk, focusing on those from LGBTQ+ and minority communities. Its efforts to increase mpox awareness and share information with the media resulted in more than 13,140 views on Instagram, Facebook, and TikTok.
Following a racially motivated massacre by a white supremacist at the Tops Supermarket in Buffalo, NY, that left 10 people dead and even more wounded in May 2022, NYHealth contributed to the Buffalo Together Community Response Fund, spearheaded by the Community Foundation for Greater Buffalo and other local funders closest to the community. By summer, initial grant funds were distributed to close to 90 Black-led organizations working in the community in the immediate aftermath of the shooting to provide food access, mental health services, and to address critical community needs.
As Ukrainian New Yorkers were and are still struggling with how to help their families in conflict zones and support family members who managed to flee the war in Ukraine, NYHealth worked with the Edith and Carl Marks Jewish Community House of Bensonhurst (JCH) to support mental health and social services for Ukrainian New Yorkers and refugees, reaching more than 3,000 arriving Ukrainians. JCH partnered with the New York Legal Assistance Group and the Urban Justice Center to screen clients at more than 180 on-site legal clinics. JCH also provided emergency assistance food cards and child-focused supports to be provided to more than 200 arriving Ukrainians in New York.
Polio made a shocking reemergence in parts of New York State in summer 2022. NYHealth worked with the Jewish Orthodox Women’s Medical Association (JOWMA) to offer community health programs and education to promote community wellness and increased vaccination rates in Rockland County and Borough Park, Brooklyn. In coordination with community partners, JOWMA will expand its community education to host monthly sessions for residents in Rockland County and bi-monthly sessions residents in Borough Park.
In October 2022, Mayor Adams declared a state of emergency as governors of Texas, Florida, and Arizona sent thousands of migrants to New York City with nothing but the clothes on their backs. Make the Road New York (MRNY) is connecting migrants with health care enrollment, health care navigation, and other specialized services, including workforce training, adult education classes, and food pantries.
Opioid Crisis
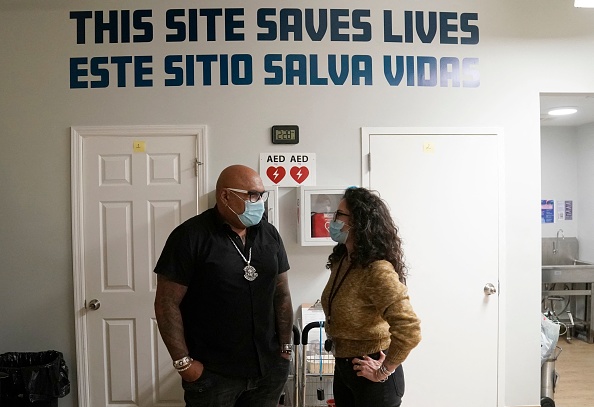
Our work to address the ongoing opioid epidemic in New York State continued in 2022. Greenwich House is piloting and evaluating a home health aide model for methadone maintenance to patients with opioid use disorder, reaching 240 eligible patients with wraparound services, including biweekly visits by home health aides. We also supported OnPoint NYC’s groundbreaking, first-in-the-nation overdose prevention centers (OPCs) in East Harlem and Washington Heights, which been used more than 42,000 times and prevented more than 600 overdoses that could have been fatal. NYHealth continues to lend our voice to raise awareness about the importance of supporting OPCs as a safe, effective, and compassionate tool to curb the consequences of the opioid epidemic.
Mental Health
The COVID-19 pandemic has exposed the need to place a greater focus on mental health in New York, especially as racially motivated attacks on Asian Americans continued in 2022. We partnered with the Asian American Federation to support the Hope Against Hate Campaign, conducting five in-language workshops to increase knowledge of the impact of racism and violence on children’s mental health. The campaign improved access to de-escalation training for close to 230 community members and supported recovery for members of the New York Asian community, including with pro bono legal services and culturally competent mental health services.
With the onset of the pandemic, children faced school shutdowns, sudden shifts to remote learning, educational loss, social isolation, fear, and trauma related to the loss of a parent or primary caregiver. The New York School-Based Health Foundation is providing technical assistance and support to 10 school-based health centers to improve detection and treatment of mental health needs among 38,000 low-income students who have returned to in-person school.
Emergency medical services (EMS) workers are also among those who have borne the acute stress of the pandemic. The Regional Emergency Medical Services Council of New York City is expanding its existing Mental Wellness Team program to 7,000 EMS workers in the City and provided training on critical incident response interventions and suicide prevention that have shown to be effective in the first responder community.
Enhancing Primary and Preventive Care
Enhancing Primary and Preventive Care
An issue of perennial importance is the need for better primary and preventive care for New Yorkers. NYHealth has been working with the Primary Care Development Corporation (PCDC) since 2020 to launch a statewide initiative to define, measure, and report on current primary care spending and increase investment in primary care services. We provided legislative testimony on rebalancing primary care, wrote commentaries on how New York must build back a better primary care system, and hosted educational events on how strengthening primary care can be a pathway to COVID-19 recovery. In 2022, the New York State Senate and Assembly enacted legislation to establish a primary care reform commission—a win for primary care and New Yorkers’ health.
NYHealth has contributed to multiple approaches to advance primary care throughout the State. The Finger Lakes Independent Practice Association (FLIPA) and the Upstate Community Health Collaborative (UCHC) merged into one IPA to bring together 18 organizations spanning 19 counties in New York State and better serve more than 200,000 patients with integrated primary care, behavioral health, and social service providers. NYHealth is supporting FLIPA to operationalize this expansion by finalizing corporate structures for a combined entity and executing new data-sharing agreements. The Auburn Community Hospital (ACH) is conducting comprehensive planning to launch a novel rural residency program that will address physician shortages and improve health care access for 78,000 rural residents in Cayuga County. The Fort Drum Regional Health Planning Organization (FDRHPO) is creating an action plan to improve access to primary care in the North Country counties of Jefferson, Lewis, and St. Lawrence. It partnered with 15 primary care provider organizations and recruited participants for 8 focus groups.
We know that primary care lies at the center of a high-functioning and equitable health care system. Our work has set the stage as we move into a new priority area focused on primary care in 2023.